“Pregnancy is a Magnesium deficient state!”
- Mildred S. Seelig, MD, MPH, FACN (1920- 2005; World-renowned Mg Expert)
http://mgwater.com/Seelig/Magnesium-Deficiency-in-the-Pathogenesis-of-Disease/preface.shtml
“Pregnancy is ‘Mt. Everest, in utero…’ “ (Barcroft, 1933)
- Sir Joseph Barcroft, PhD, CBE, FRS (1872 – 1947)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4728207/
As an opening volley, much of what you know or think you know about pregnancy is, at best, incomplete. A bold and unsettling assertion, but then I’m no stranger for taking on the tsunami of conventional medicine and proving that they are not just “wrong,” but more often than not, 180 degrees out of sync with nature. This Iron Toxicity Post will be no less controversial, and no less based on scientific intelligence and integrity.
Buckle up!… It’s going to be a rough ride…
This Iron Toxicity Post obviously builds on the popular series “You Are NOT Anemic!” and redirects the spotlight on “anemia of pregnancy,” which is a condition that is totally misunderstood, and myth-treated in the world of conventional obstetrics and midwifery. It is as though Birthing professionals have never heard of, nor understood the natural concept of “hemodilution” that occurs during the course of pregnancy.
How I became aware of, and more significantly, obsessed with this metabolic confusion, is an issue that still eludes me. As one of my physician colleagues observed recently, “This is an integrity issue for you, isn’t it?”. Damn straight it is! The human fetus is the most defenseless being on the planet. They need our passion and our protection.
For those that don’t know by now, my “PhD” stands for “Passionate hatred for Deception”.
What we can all agree on is that women have been giving birth to babies for millennia of millennia.
It is a gradual, eventual, transformational, painful, but altogether, natural process. No. I have never given birth, but I have been blessed to witness and participate in the birth of each of my four amazing children. Truth be known, I wish that I knew then what I know now. But alas, I didn’t, and now I want to share some vital pearls of mineral wisdom with women who are in the throes of growing and giving birth to the next generation of humanity.
As I noted above, the child in your womb is the most defenseless and vulnerable species on our planet. It is time we had more accurate information on the maternal metabolic dynamics that are in play in your bodies. We are going to cover three key topics in this post:
- The hypoxia-driven state of pregnancy, that causes magnesium loss and drives proliferation
- The amazing Cupro {copper} dynamics of key enzymes that run and regulate pregnancy dynamics
- The absolute fact that Mother Nature expects your hemoglobin to drop in the last trimester
On a broader level, it is important to know that we are being trained (triggered?) to react impulsively to this “deficiency”, or that “excess”, as though our human metabolism were some GIANT “gas gauge” that only registered “High” and “Low”. Please understand, most metabolic pathways are assessed by a gauge that is more akin to “Miles Per Gallon” – not a grade-school “dipstick!” I’m curious, when was the last time that adding more gas improved your MPG (Miles Per Gallon)? Hmm? This flawed mindset applies to calcium, vitamin-D, hormones, most nutrients, and yes, IRON, most of all.
Have you ever wondered why you were never told to add magnesium, vitamin-A and copper? And have you ever noticed that these latter three nutrients are never on the nutrient tables assigned to the foods we buy and eat? Do you think that that’s an oversight, or possibly by design. As a friend once said, when the government is consistently wrong, it must be by design.
In any event, please forgive the bunny trail there, let’s get back to the ever-expanding story on the planet!
Hypoxia of Pregnancy:
Sir Joseph Barcroft was a British physiologist that was fascinated by the physiology of alpinists and mountain climbers. He made enormous contributions to this field during the opening decades of his distinguished career. But in his later years, he turned his attention to an equally “hypoxic” experience – pregnancy!
https://link.springer.com/article/10.1007/s40495-016-0050-5
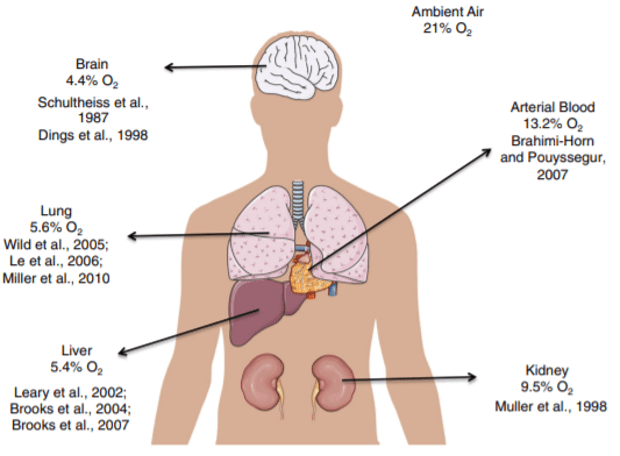
As is evident above, the partial pressure of Oxygen (pO2) in the air we breathe is ~21%. Nitrogen is ~78% of that same air…and this (pO2) drops as it gets distributed to various organs around the body, as noted in the diagram above. And why is this important?
The oxygen concentration in the womb in the 1st trimester of pregnancy is ~1-3% — which is hypoxic! (i.e., “anaerobic!” which requires magnesium to produce energy). What is critical to understand is that there is high proliferation of tissue in an anaerobic environment.
The oxygen concentration in the womb in the 3rd trimester of pregnancy is ~5-8% — which is normoxic! (i.e., “aerobic!” which requires copper to produce energy). What is equally critical to understand is that there is high differentiation of tissue in an aerobic environment.
As you reflect on what’s happening metabolically throughout the course of the pregnancy, these differences and changes make perfect sense.
An interesting article that speaks to these oxygen-related dynamics in pregnancy is noted below:
https://pubmed.ncbi.nlm.nih.gov/28395175/
Please NOTE, conventional obstetrical practices measure neither mineral. Now the opening quotations by those two gifted scientists and clinicians make a bit more sense. What should unsettle you, however, is how little attention is placed on the following dynamics in the course of a typical pregnancy:
- Mineral metabolism,
- Oxygen metabolism and
- Energy metabolism.
Truth be known, women who are pregnant have an anaerobic parasite growing inside their aerobic being. And the mineral, oxygen and energy dynamics are completely different in these two organisms.
Two important articles that underscore the importance of these minerals are the following studies:
- Suliburska et al, 2016, “Concentrations of Mineral in Amniotic Fluid and Their Relations to Selected Maternal and Fetal Parameters”
https://therootcauseprotocol.com/wp-content/uploads/2022/10/Concentrations-of-Mineral-in-Amniotic-Fluid-and-Their-Relations-to-Selected-Maternal-and-Fetal-Parameters80.pdf
If you take the time to read this important study from Poland, you will discover just how essential magnesium and copper are to the developing fetus. Again, there is no routing assessment of either mineral in standard obstetrical practices. - Gambling L, McArdle HJ, 2004, “Iron, copper and fetal development”
Abstract: https://pubmed.ncbi.nlm.nih.gov/15831127/
FULL: https://www.researchgate.net/publication/7906238_Iron_copper_and_fetal_development
As you look over the abstract, you will note that Dr. McArdle, a world-renowned researcher is hardly alone in studying not just iron, but also copper requirements in proper fetal development. It begs the obvious question, where is this focus in conventional obstetrical and midwifery training. Why is there NO mention of copper status? We will see that this is a particularly important issue in the next section.
Maybe an important question is to ask how these mineral’s assessments might be incorporated into routine obstetric check-ups.
Metabolic dynamics and key copper enzymes:
A glaring oversight of conventional obstetrics, imho, is the fact that copper and iron dynamics are central to oxygen transport, energy dynamics, metabolic and structural development, to name but a few factors, not the least of which is the actual transfer and regulation of these metals between mother and fetus.
What is important to understand is that there are three KEY enzymes (engines) that are regulating the flow and dynamics of these metals:
- Ceruloplasmin,
- Hephaestin, and
- Zyklo-WHO?!?…
It is absolutely stunning to me that these critical metalloenzymes are not routinely assessed as part of a normal obstetrics check-up. They have a profound role to play in the proper, normal and natural transfer of copper and iron between the players. They are at the forefront of oxygen <> energy metabolism. They are MIA in obstetrics practices.
Kuo, McArdle et al, 2007, “Zyklopen, a new member of the multi-copper ferroxidase family, is expressed in multiple tissues”
Chen, McArdle et al, 2010, “Identification of Zyklopen, a New Member of the Vertebrate Multicopper Ferroxidase Family, and Characterization in Rodents and Human Cells”
Wierzbicka et al, 2014, “Ceruloplasmin, hephaestin and zyklopen: the three multicopper oxidases important for human iron metabolism”
https://journals.indexcopernicus.com/search/article?articleId=55806
Gambling L, Kennedy C & McArdle HJ, 2011, “Iron and copper in fetal development”
https://pubmed.ncbi.nlm.nih.gov/21893209/
Trust me, there are many, many other articles that speak to these mineral dynamics and the role that these key enzymes play in running and regulating the optimal placement and management of these metals. You are totally unaware of their existence and their importance because your birthing practitioner is totally unaware of them, as well… Please understand, my goal is educate and enlighten, not add to the nausea that you might be experiencing due to the presence of that “parasite!”
Maybe another important question is to ask how these key enzyme’s assessments might be incorporated into routine obstetric check-ups.
You are NOT “Anemic!”:
It is a known biological fact that all mammals experience a drop in hemoglobin during the 2nd half of the pregnancy. It is the natural order of this process.
Sometime around the 1st World War, the League of Nations (precursor to the U.N.) did a study of iron status in society and “discovered” that pregnant women, representing ~1% of society, were “anemic!” – as they should be. But this “perceived deficiency” was turned into a “condition,” and the world has never been the same since.
This so-called “anemia” was the basis for the iron fortification programs that started at the outset of the 2nd World War. Yes, they decided to “inoculate” the 99% of society that was not pregnant to ensure that there would be no iron deficiency in society. Of course this makes no sense but that is what drove that dietary supplementation.
An absolutely essential study to read to refute these conclusions is the pioneering and penetrating research of Philip J. Steer, MD, et al, 1995, “Relation between maternal haemoglobin concentration and birth weight in different ethnic groups”.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2548871/
If you do nothing else as a result of reading this post, please read this important study!
Please share it with your birthing practitioner. They are not aware of this information and why is this SO important? Dr. Steer and colleagues examined 150,000 live births in England to assess the correlation between mother’s hemoglobin (Hgb) status and baby’s birth weight – a sign of a healthy new born.
What they learned, which is vital to this post, is the following:
Non-pregnant women’s Hgb: 12.5 – 13.5 mg/dL
Pregnant women’s Hgb in 1st Half of Pregnancy: 12.5 – 13.5 mg/dL
Pregnant women’s Hgb in 2nd Half of Pregnancy: 8.5 – 9.5 mg/dL
That is an enormous change in hemoglobin status and given that hemoglobin represents ~70% of the body’s iron status, this is the only marker that should be used. Imho, serum ferritin levels are not relevant to “iron status” during pregnancy. What is critical to understand is that there is a complete lack of awareness and understanding of this seminal research in the world of obstetrics. This is quite alarming to me.
Now, that is the experiential side of this issue. In actual practice, in a rigorous study, the mother’s Hgb was found to be much lower than is considered “safe and/or healthy” in today’s world of obstetrics. Lower Hgb is the driver for a healthier baby. Unfortunately, this lower Hgb is also considered the driver for greater blood loss during the course of delivery.
Thus, there is a conflict in the training of birthing practitioners. The decided emphasis is upon increasing iron status – as measured by Hgb – which is known to affect the baby’s health status and is suspected to improve the chances of lower blood loss. And it turns out that this latter issue is a case of mistaken dynamics that iron and copper play in the microcirculation, which is where “hemostasis” (stemming the blood loss) actually takes place. It is safe to conclude that practitioners are trained that iron is key, and given the paucity – the almost total lack of any copper awareness – they are not being trained in the vital and central roles that bioavailable copper plays in stopping blood loss.
It is a fascinating aspect of copper metabolism that could easily consume a textbook. Alas, we haven’t the time for that, now do we?
SUMMARY POINTS…
The key is buried in an important article that I stumbled upon, Schuschke DA, 1997, Dietary Copper in the Physiology of the Microcirculation
To give you a sense of its importance of this article by Dr. Schuschke, it is one of the ten most important articles that I have read in 11 years (6,000+ and counting) Have I got your attention, now?
Here is the key Sentence from Schuschke, 1997:
“Because erythrocytes [RBCs] enhance platelet activity (Santos et al, 1991 —below) the low hematocrit [emphasis added] may be a mechanism for the inhibited hemostasis.”
https://pubmed.ncbi.nlm.nih.gov/1991840/
An important consideration: Do Cardiologists, Cardiovascular Surgeons and Interventional Radiologists see the solution the same way? Of course they don’t!!! There is a vast difference between using a pill, a scalpel and a stent to solve a coronary blockage!
And this Santos article provides a Hematologist’s point of view. Schuschke provides a detailed perspective from a “Mineralist’s” point of view! And what Dr. Schuschke profiles — in detail — is the profound importance of bioavailable copper to healthy, natural thrombogenesis and hemostasis. Again, these are clinical terms that speak to the formation of “clots” and “stopping the blood flow”. And again, there is no mention of copper metabolism in birth practitioner training!
Key Insights from having read, and reflected extensively on these articles:
KEY INSIGHT #1:
Low hepatic copper = HIGH hemorrhaging and increased bleeding time (Schuschke et al, 1995b). Profoundly important correlation.
KEY INSIGHT #2:
There are 3 key factors in homeostasis:
- Activation of platelets
- Aggregation of platelets, and
- Adhesion of platelets to endothelial cells
Copper deficiency affects both Thromboxane (TxA2) and von Willebrand Factor (vWF) that are key to bringing about homeostasis:
- Copper deficiency increases TxA2 to increase activation and aggregation.
- Copper deficiency decreases vWF to slow/prevent adhesion of the aggregated platelets! VWF is Copper-dependent vWF is MIA in obstetrics! This is a stunning and glaring defect of obstetrics!
KEY INSIGHT #3:
Lack of bioavailable copper destroys the natural structure and function of the microcirculation!
- Lack of BH4 (Folate is copper dependent) lowers NOS function and thus, production of NO• {Nitric Oxide}
- Lack of CuZnSOD (copper dependent) increasesO2- that destroys availability of NO•
- Lack of copper prevents both:
- NO•-Heme binding in GC-S (soluble Guanylate Cyclase)
- NO• Activation of GC-S!
(These critical concepts are profiled in Fig 5 of Schuschke, 1997)
- Lack of copper also destroys lysyl oxidase enzyme that is also involved in wound repair…
- Lack of copper weakens the energy/ATP production and “intelligence” of endothelial cells, which are active participants in any hemostasis process!
But Morley, what are the non-scientific BIG TAKEAWAYS I need to get from these key insights?
For the vast majority of those reading this right now, the above key insights may be leading you to scratch your head and try to stretch back to biology and chemistry of many years ago… don’t worry, you likely didn’t know much of these then, and your healthcare providers probably haven’t been taught about them either, but what you CAN do from now becoming aware of these aspects is considering learning more about the Root Cause Protocol (RCP) and look at adding sources of bioavailable copper, retinol, magnesium and adrenal support as a part of that process. Talk to a RCP Consultant if you want to have guidance through this process.
It boils down to this…
Pregnant women NEED bioavailable copper. Lack of bioavailable copper is a HUGE problem when pregnant for the health of mother and baby. The majority of humans do not have enough bioavailable copper, and without a focused effort from a variety of angles, it’s difficult to support this aspect of our metabolism, especially after most of us have many years (if not a lifetime) of not having sufficient for ourselves, let alone our babies.
Now, I realize that this was a somewhat broad and sweeping treatment of some key factors in obstetrics. I could easily turn this post into a book and will likely do that in the not too distant future.
What I want you all to understand is that there is way more to a healthy, uneventful pregnancy and delivery than a robotic focus on iron and vitamin-D status. Know that both of these ubiquitous and contemporary “nutrient darlings” are known to kill the ability to produce bioavailable copper. No, it is unlikely that your birthing practitioner knows that. They are merely doing what they have been trained (“scripted”) to do. Nothing more and nothing less.
The raging and alarming rise of autism in society today (unheard of in 1930 and today it affects 1:34 infants) alone should make you question what has changed in our general environment and what has changed in the obstetrical environment. The overriding obsession on iron and vitamin-D status – neither of which is found in mammalian breast milk – should give you pause to step back and reflect on what is really driving these “D”ictums
There is much more to this story, but you now have some key facts and dynamics that will empower you to think differently about this natural biological process and hopefully ask better questions, gain better answers and ultimately make better, and more healthy decisions for you and your defenseless fetus that is growing inside your womb.
A votre sante!
MORLEY M. ROBBINS
