Iron Toxicity Post #52
In my continuing efforts to “take off the gloves,” about how they are being poisoned by iron fortification, iron supplementation, iron infusions, iron stimulation, iron mesmerisation, etc. Today’s post will present some new dimensions to this iron discussion that will hopefully “stimulate your little grey cells”, as the great fictional and enigmatic detective, Hercule Poirot, so frequently said while solving equally perplexing, yet elusive, murder mysteries.
One of my clients suggested that I might find this blog on curcumin and iron useful:
margaret.healthblogs.org/life-with-myeloma/discovery-of-curcumin/curcumin-and-iron/
In fact, it’s quite good, it’s well written, but it is quite misleading. Nevertheless, this blog rocked my world, and I am grateful to Margaret for that!
I’ve read a couple hundred articles on iron, iron metabolism and iron dysregulation. I also read my fair share of articles on ferritin, and yes, I knew that ferritin came in two forms: an active state (heavy-ferritin with ferroxidase function) and an inactive state (light-ferritin without this enzyme function). I hadn’t shared that bombshell as of yet, but did any of you know that ferritin had two forms?
I really wonder now, are we low in the active or the inactive state of ferritin?
But what this Blogger, Margaret, wrote that really caught my eye is the fact that ferritin has a relationship to both iron and oxygen!
Oxygen? How, exactly, did I miss that functional factoid? Given that ferroxidase has a special relationship with oxygen, wouldn’t it be best to have the heavy (active) ferritin form? I wonder how many healthcare providers are aware of these important iron dynamics?
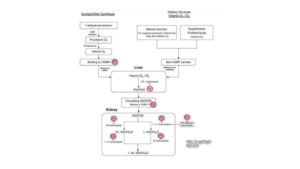
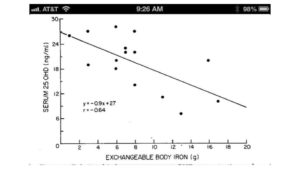
Liu, X., et al. (2006). “Iron at the center of ferritin, metal/oxygen homeostasis and novel dietary strategies.”
www.scielo.cl/pdf/bres/v39n1/art18.pdf
Theil, E.C. (2003). “Ferritin: At the Crossroads of Iron and Oxygen Metabolism.”
It turns out that iron is actually a Janus – it wears two faces across numerous dimensions. Here are some critical and dualistic facts about iron:
- Iron comes in two oxidative states: ferrous (Fe2+, soluble) vs. ferric (Fe3+, insoluble)
- Ceruloplasmin comes in two forms: ferroxidase enzyme vs. immuno-reactive protein
- Ferritin, as noted above comes in two forms: H-ferritin (active) vs. L-ferritin (inactive)
- Iron has two roles with oxygen: carrier of oxygen (Hemoglobin) vs. creator of oxygen radicals (reactive oxygen species)
- Iron dysregulation comes in two forms: “anemia of iron deficiency” (very rare!) vs. “anemia of chronic inflammation” which I believe is pandemic on this planet
- Iron metabolism has two dimensions: Iron metabolism vs. Copper<>Iron metabolism
- Copper has two oxidative states, as well: cupric (Cu+) vs. cuprous (Cu++)
Now you can understand how I feel about iron anemia vs. iron dysregulation and practitioners’ use of high and low to describe our iron status is very misleading!
The worlds of medicine, nutrition and mineral metabolism are littered with this “High” vs. “Low” mentality. It is criminal, and it is the very origin of how we’ve gotten so confused about iron and have become so iron toxic!
There is no such thing as iron metabolism.
For a fact, it is copper<>iron metabolism, the leading researchers know this, and point out that these two metals are joined at the hip of ceruloplasmin (Cp). This Cu<>Fe metabolism is actually a Ventriloquist Act, which means iron is the dummy.
It is not all about how much iron; it’s all about how usable is it. We are learning that ferritin can be most unusable especially when ferritin is in the Light-ferritin form.
I have come to reflect on it, ferritin is the ultimate Trojan horse, especially in a body that lacks ferroxidase function in its ceruloplasmin, as well as in its ferritin.
We all know that horses are most useful when they are functional? Well, this is true of iron, and ferritin, too!
The inactive “Trojan ferritin” being fed more iron is simply adding insult to your non-functional iron pool, especially if your mag RBC and serum ceruloplasmin are both anemic.
So, if you still have a mind to think that you’re “anemic”, even after all this post. Please take this little test to assess your indications of iron knowledge.
- Do you still think anemic only means a lack of iron?
- Do you still believe your healthcare provider understands the Janus duality of iron, as noted and outlined above?
- Do you still use the redundant terms “high” and “low” to describe your dysfunctional iron and your dysfunctional ferritin status?
- Do you still not understand what “anemia of chronic inflammation” is referring to?
- Have you still not gotten the Full Monty Iron panel, nor had it properly interpreted?
- Have you still not taken the time to view, nor reflect on the Root Cause Video?
- Have you still not started to adopt the Stops and Starts of the Root Cause Protocol?
- Have you still not stopped taking multi-vitamins/iron supplements/iron infusions?
- Do you still continue to research what the signs and symptoms of “anemia” are on the Internet?
- Have you still not read any of the 50+ posts on iron toxicity?
- Have you still not questioned your doctor’s understanding of the Janus duality of iron?
If you say yes to any of the above questions, then you are still following iron anemia rather than iron/copper metabolism.
What I am noting in more and more iron research articles, are increasing references to the term “Iron deficiency” being openly referred to as the “lack of functional iron”. Not an absolute “deficiency of iron!” Big difference!
Copper<>Iron metabolism is all about making the iron functional. That is only possible with the presence and prevalence of copper and copper-driven enzymes like ceruloplasmin (Cp). Also the copper dependent anti-oxidant enzymes (SOD, CAT, & GPx) designed to neutralize the iron-driven reactive oxygen species (ROS) that unbound iron creates with no limits within our bodies, our tissues, and our cells.
If your healthcare practitioner(s) are not questioning your true iron status and are not focusing on your magnesium and ceruloplasmin status. Then treating you with calcium, hormone-D, zinc and iron. And worst of all, are still “attacking” your alleged “copper toxicity,” then they are not addressing your body’s core needs or honoring its innate healing potential.
This duality of iron is very poorly understood! The systemic simplistic solution of adding more iron to your iron dysfunction is both one-sided and dangerous.
Here is a great way to start the process of better understanding your iron status, as well as supporting its recovery and rebalance within your body:
https://therootcauseprotocol.com/about/
A votre sante!
Morley M Robbins
For Facebook Discussion:
https://www.facebook.com/groups/MagnesiumAdvocacy/permalink/1261433993924667/