Osteoporosis and Estrogen/Hormones – what’s the link?
We already know from several past iron toxicity posts that hormones are ruled by enzymes that RELY on minerals for activation in the body – so, if our adrenals aren’t working effectively (stress anyone?), the body goes into a ‘backup mode’ and changes happen in the hormones (Estrogen Dominance so often rolls on in! What is now known is that the estrogen is not low, but simply not bioavailable. Sound familiar?)
And what’s underlying these habitual, and all-too-common hormonal changes? Once again, excess, unbound iron!
There is discussion in the paper by Jian J, Pelle E, Huang X., 2009, about the involvement of hormones, including estrogen, in osteoporosis.
“……In addition to Estrogen deficiency, abnormally high iron is a key cause of postmenopausal osteoporosis.”
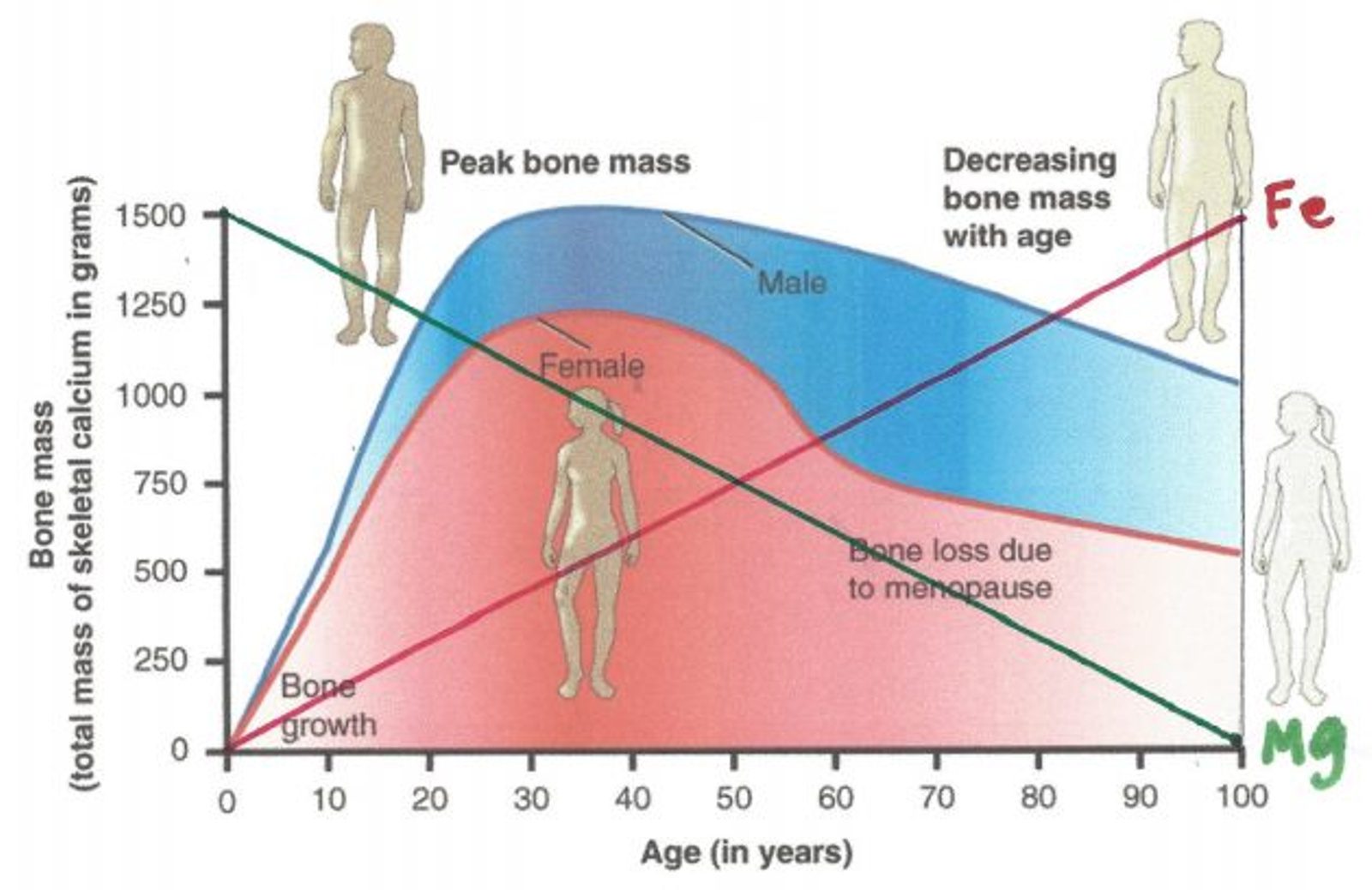
So, are you telling me that if we have women experiencing Estrogen deficiency, then abnormally high iron is a key player in osteoporosis as a result? What? Hormones are related to bone density?
How many more MAG members just pricked up their ears?
I would suggest considering the other ‘book end’ of Estrogen Dominance having an involvement there, too – as has been talked about extensively in past iron toxicity posts/discussions in MAG. Instead of obviously high Iron by the definitions commonly used, we know that iron stores are building, while the amount of ‘available’ and ‘usable’ iron is dropping; bioavailable copper and magnesium are bottoming out. The true iron levels are not obvious particularly because of the testing generally done by conventionally trained practitioners.
Underlying the Estrogen Dominance – there is still excess, unbound iron wreaking havoc in the woman’s body, preventing bone regeneration and seeing bone density dropping rapidly, especially when women become post-menopausal.
(Which leads to ↑ Iron via supplementation in allopathic and other conventional practitioner circles and ↑ estrogen, and ↑ risk for Osteoporosis!)
More iron loading, more Estrogen Dominance problems, more drugs and synthetic hormones added to their body to ‘fix’ the problem (i.e. ‘treat the seats’ of symptoms) and the sicker female folks get.
Huo Y et al, 2012 comment within their article “Excess iron is associated with various diseases including osteopenia and osteoporosis, which are closely related to the alternation of the endogenous estrogen level”. They talked about creating a mouse model by removing ovaries and then monitoring hemoglobin and serum iron (both decreased) yet the iron level in the liver and spleen tissue increased. Hepcidin was elevated in these mice too.
When was the last time your doctor tested your hepcidin levels if they were worried about anemia?
Stick with me here a bit longer here- if Estrogen contributes to iron homeostasis, and we have a stressed out population of women who have been misled and misfed information about what is really in their food, what is in their birth control pills, they have led a low-fat (i.e. low Retinol-A, low-bioavailable copper) diet, eaten less and less of the foods their parents (Mothers) and grandparents (grand-Mothers) ate potentially more laden with sprays and processed food than previous generations.
You mean to tell me that when post-menopausal, there are signs that it’s likely more Iron will be stored via Hepcidin in the organs, while the amount of iron in their hemoglobin and serum drop. What? Does this sound familiar to any of you reading along?
Not to mention that we have a population where more and more women are having symptoms of or labels applied of estrogen dominance – so many either being thrown into surgical menopause (often not keeping ovaries too!) or due to other imbalances.
Now let’s build our list…
↑ Excess Iron = ↑ Oxidative stress = ↓ osteoblast regrowth = less bone density
↑ Excess, unbound iron = ↑ Estrogen = ↑ Iron stored into the Liver via Hepcidin + ↓ levels of Hemoglobin + Serum Fe
Osteoporosis and retinol – how can it help?
I have recently discussed the critical importance of Retinol in our bodies to help get the body moving Iron where it needs to go, getting our Bioavailable Copper increased, and so much more.
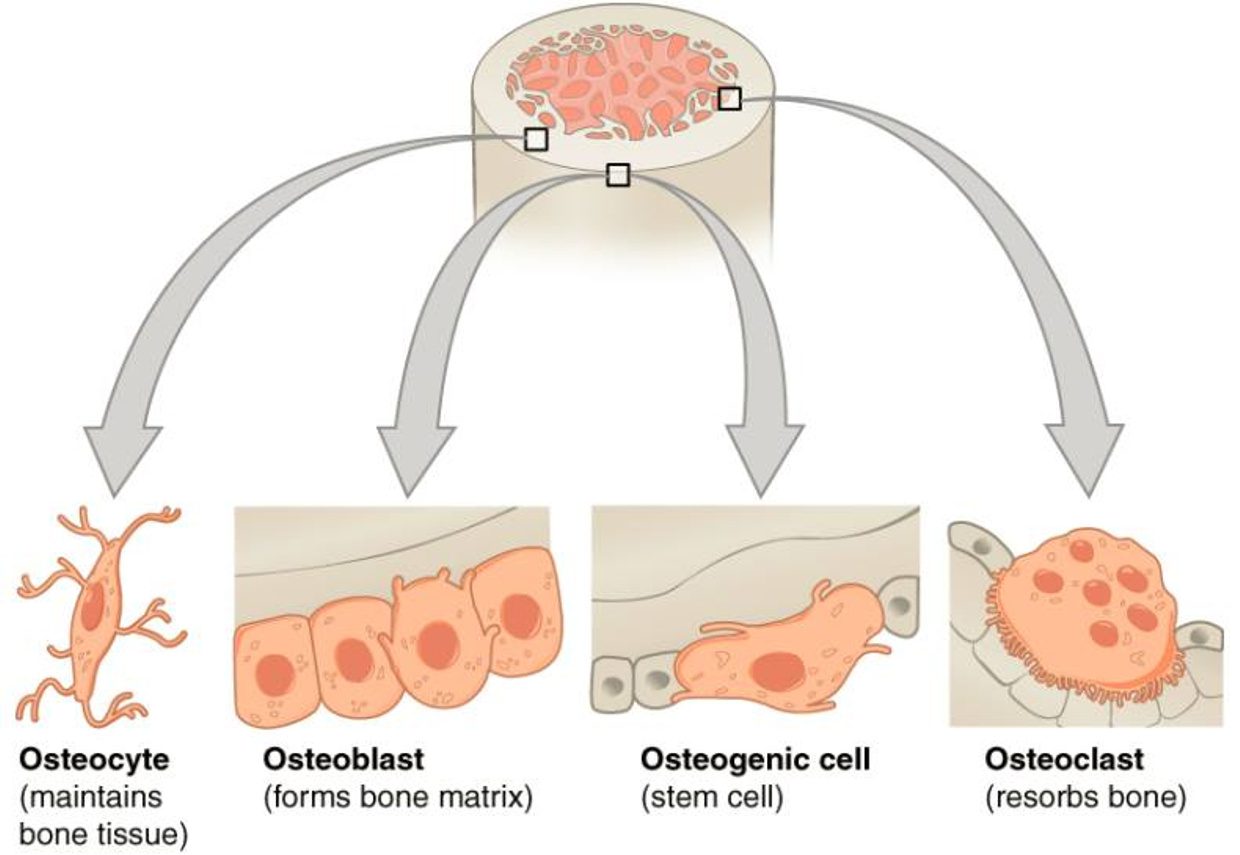
We know that new blood cells are made within the bone marrow (or the cascade of cell creation is started there at a minimum). We are learning today that when there is high oxidative stress as iron increases in the body, that the regeneration of bone cells (osteoblast regeneration) is reduced.
What else do the osteoblasts need to carry out the repair and regeneration? Three key Ingredients:
Retinol-A (Vitamin A), Bioavailable copper and Magnesium
Bloem, 1995 stated that ‘repletion with vitamin A was followed by regeneration of the bone marrow, disappearance of the Hemosiderin from the spleen and liver, and erythroblastic activity.’ That’s a BLOCKBUSTER SHIFT in the dynamics of bone activity, btw.
We have established above that there’s more iron getting stored into many women’s livers and spleens from hormone imbalances, that with increased oxidative stress, there’s less osteoblast regrowth in the bones and less bone density and now we are saying that retinol (vitamin a) intake from food causes regeneration of bone marrow, reduction in the loading of iron in the spleen and liver, and increased cell production?
No way?
What’s compounding these changes? ‘Stressors!’ (From our very stressful modern day life, from the chemicals put into our bodies, food, inherited from our mothers/ grandmothers, from blue light bombardment, from expectations of mothers to be everything to everyone 24/7, from excess, unbound iron, the never-ending process of creating oxidative stress keeps chugging it out!)
Back to our list…
↑ Excess, unbound Iron = ↑ Oxidative stress = ↓ Osteoblast regrowth = LESS bone density
↑ Excess iron = ↑ Estrogen = ↑ more Iron stored into the Liver via Hepcidin + ↓ Hemoglobin + Serum Fe
↑ Retinol-A (via food repletion) = ↑ bone marrow regeneration = ↑ Osteoblasts (maintain bone density) + ↑ new blood cells = ↑ Ferroxidase activity = ↓ Excess, unbound iron = ↓ Oxidative Stress
Vitamin D, zinc and calcium supplementation – why aren’t these critical to bone strength as we keep getting told?
We are already starting to see a picture on how come the RCP (Root Cause Protocol) ties in with reducing the chances of osteoporosis, reduce excess unbound iron, decrease oxidative stress via adrenal support and magnesium, increase bioavailable copper and retinol through food/whole food supplements, and we have our bases covered for the true osteoporosis risk factors.
So how about the Vitamin D (Hormone-D!), K2, zinc and calcium side of things?
These have been addressed – ad nauseum — by previous posts, but here’s a quick summary.
– We get K2, zinc and calcium from eating an ancestral diet, which is as wide and varied as possible.
– We get Hormone-D from sunlight and foods such as eggs and cod liver oil (both great sources of retinol – who would have thought??).
– Calcium carbonate supplements (most commonly suggested) require 12 steps to metabolize them into a form we can actually use. Other than many of the population not having the energy/mineral reserves to deal with that, many of us are going to grind to a halt (think cement = calcium) if calcium is supplemented from anything except food
– Supplemental Hormone D kills retinol/retinoic acid in our liver, eyes (see iron toxicity post #62) and elsewhere in the body, preventing it from being able to facilitate cellular regeneration, repair and renewal, leading to a weakening in bone strength and repair.
– Excess hepatic iron disrupts the 25(OH) enzyme (also mag dependent) – if we have excess iron in our liver and we don’t have enough magnesium, we can’t carry out the transfer of Hormone D within the body – so it’ll test ‘low’.
– What’s the biggest reason for insufficient zinc in the body? Excess unbound iron.
– Did you know: Magnesium from food and suggested supplemental sources helps the calcium to go where it’s needed?
We need bioavailable copper (Evans et al, 1970) and retinol to synthesize ceruloplasmin – And it turns out that Retinol-A is absolutely critical to loading that ^^^^ Copper to ensure Ferroxidase (FOX) enzyme function (Barber & Cousins, 1987)
If we have insufficient Retinol-A, and a lack of magnesium and a lack of Bioavailable Copper, what happens? We don’t have enough ferroxidase function, and we are faced with Iron that is dysregulated and prone to act out!
What else happens when we don’t have enough ferroxidase function?
We build up excess stored iron, yet apparent low blood Iron (because the body wants to protect us from the massive oxidative stress that high or hiding Iron in the blood represents) our adrenals get stressed out, we start to get any number of metabolic ‘conditions’ kicking in – hormonal imbalances, autoimmune conditions, diabetes, arthritis, depression, Alzheimer’s, our healthcare practitioners tend to dish out more iron, Vitamin-D and any number of other medications which only compound and confuse these conditions!
Now the way the RCP (Root Cause Protocol) looks at these things is dramatically different.
Look at our expanded list now!
↑ excess Iron = ↑ Oxidative Stress = ↓ Osteoblast regrowth = LESS bone density
↑ excess Iron = ↑ Estrogen = ↑ more Iron stored into the Liver via Hepcidin + ↓ Hemoglobin + Serum Fe
↑ Retinol (via food repletion) = ↑ Bone Marrow Regeneration = ↑ Osteoblasts (maintain bone density) + ↑ New blood cells = ↑ Ferroxidase enzyme function = ↓ Excess, unbound iron = ↓ Oxidative Stress
↑ Magnesium + Bioavailable Copper + Retinol-A = ↓ Oxidative Stress including ↓ Excess, unbound Iron = less chance of osteoporosis/osteopenia (and the added bonus that Hormone-D will stabilize, too, in general!)
What does all this really mean? Just tell me how to reverse this osteoporosis risk.
The research behind the RCP (Root Cause Protocol) has always been encouraging the consumption of whole foods to obtain whole food vitamin c (to help with bioavailable copper), magnesium and adrenal support (to reduce stress on the body and provide important components for making Mg-ATP (energy)) and retinol (vitamin A).
The research shared today is emphasizing that this is the right path, and that if you want strong bones, low risks of fractures, and to reduce the chance of getting osteoporosis. Do the protocol!
¬ Reduce your oxidative stress (from food, physical/mental stress, get plenty of sleep, etc).
¬ Increase your retinol-A, Bioavailable Copper and Magnesium to give you more energy, reduce inflammation and give your body a chance to heal itself
¬ Release stresses of the past and emotions, which may be holding you, back from progressing.
¬ Reduce your iron load (when ready – support your body before donating blood!)
RCP = ↓ oxidative stress + ↑ via Bioavailable Copper, Mag, Retinol-A = ↓ Excess, unbound Iron = ↓ chance for osteoporosis AND better mineral flow throughout the body as well as ↑ positive health outcomes (= DEC ↓ “Stress!”)
Let’s go with the simplicity of eating real food, whole food supplements and reducing “Stress!” in our life of all forms, rather than getting too lost in the enormity of the deception which has been around us on this and so many other topics we cover in this MAG FB Group (https://www.facebook.com/groups/MagnesiumAdvocacy)! The deception is very real, but the effort to ‘fight it!’ is simply not worth the expended MBR (Mag Burn Rate) associated with that effort!
So here’s to a Happy Mother’s Day to all of the Moms, Mums, Grannies, Grandmothers, etc. that have allowed us all to be here, to be apart of this grand experience called Planet Earth! Most of all, thank you for the love and patience that you have shared and taught us, and may we enrich the lives of those around us – whether related or not — with the mineral truths and insights that are regularly being shared on this MAG FB Group (https://www.facebook.com/groups/MagnesiumAdvocacy).
A votre sante!
MORLEY M. ROBBINS
References within or relevant to Iron Toxicity Post #70
Christenson RH. 1997. “Biochemical markers of bone metabolism: an overview.” Clin Biochem 30:573–593. www.ncbi.nlm.nih.gov/pubmed/9455610
Zarjou A et al, 2010, “Ferritin ferroxidase activity: a potent inhibitor of osteogenesis.” (www.ncbi.nlm.nih.gov/pubmed/19821764 )
Weinberg ED, 2009-July, “Iron Loading in humans: a risk factor for enhanced mortality & morbidity.
”https://www.researchgate.net/publication/232033197_Iron_loading_in_humans_A_risk_factor_for_enhanced_morbidity_and_mortality
Weinberg ED, 2008, “Role of Iron in Osteoporosis” (Abstract ONLY) www.ncbi.nlm.nih.gov/pubmed/19337160
Jia P et al, 2012, “Ferric Iron Could Facilitate Osteoclast Differentiation & Bone Resorption thru ROS” onlinelibrary.wiley.com/doi/pdf/10.1002/jor.22133
Yamasaki K, Hagiwara H. 2009, “Excess iron inhibits osteoblast metabolism” www.ncbi.nlm.nih.gov/pubmed/19735707
Jian J et al, 2009-Dec, “Iron & Menopause: Does Inc Iron Affect the Health of Postmenopausal Women?” www.ncbi.nlm.nih.gov/pmc/articles/PMC2821138/
Cervellati C et al, 2014 “Oxidative Stress and Bone Resorption Interplay as a Possible Trigger for Postmenopausal Osteoporosis”
www.ncbi.nlm.nih.gov/pmc/articles/PMC3913453/
Rossi F et al, 2014-Dec, “Iron overload causes osteoporosis in thalassemia major patients through interaction with transient receptor potential vanilloid type 1 (TRPV1) channels”
www.ncbi.nlm.nih.gov/pmc/articles/PMC4258755/
Xiao W et al, 2015-Sept, “Iron overload increases osteoclastogenesis and aggravates the effects of ovariectomy on bone mass”
https://joe.bioscientifica.com/view/journals/joe/226/3/121.xml
Cervellati C et al, 2014 “Oxidative Stress and Bone Resorption Interplay as a Possible Trigger for Postmenopausal Osteoporosis”
www.ncbi.nlm.nih.gov/pmc/articles/PMC3913453/
Jian J, Pelle E, Huang X. 2009. “Iron and menopause: does increased iron affect the health of postmenopausal women?” Antioxid Redox Signal 11:2939–2943.
Hou Y et al, 2012, “Estrogen Regulates Iron Homeostasis through governing Hepatic Hepcidin expression via an estrogen response element”
https://www.sciencedirect.com/science/article/abs/pii/S0378111912011699
Barber EF & Cousins RJ, 1987, “Induction of Cp Synthesis by Retinoic Acid in Rats–Inf of Dietary Copper & Retinoic” Acid_JrlNutrition www.ncbi.nlm.nih.gov/m/pubmed/3655940/
Guggenbuhl P, Deugnier Y, Boisdet JF, et al. 2005, “Bone mineral density in men with genetic hemochromatosis and HFE gene mutation.” Osteoporos Int 16:1809–1814 (www.ncbi.nlm.nih.gov/pubmed/15928800)
For Facebook Discussion
www.facebook.com/groups/MagnesiumAdvocacy/permalink/1708813685853360/